Have you ever heard of the remarkable role that your pelvic floor plays in your daily life? These often-overlooked muscles have a significant impact on our well-being, affecting everything from bladder control and digestion to sexual function and core stability. When these muscles aren’t functioning optimally, it can lead to discomfort, pain, and a host of other issues. That’s where internal pelvic floor physical therapy comes into play. In this article, we’ll delve into the world of internal pelvic floor therapy, exploring its benefits, techniques, misconceptions, and more.
Contents
- 1 Understanding the Pelvic Floor
- 2 When is Internal Pelvic Floor Physical Therapy Needed?
- 3 The Role of a Pelvic Floor Physical Therapist
- 4 Benefits of Internal Pelvic Floor Physical Therapy
- 5 What to Expect During a Session
- 6 Pelvic Floor Exercises and Techniques
- 7 Preparing for Your First Appointment
- 8 Conclusion
Understanding the Pelvic Floor
The pelvic floor refers to a group of muscles, ligaments, and connective tissues located at the base of the pelvis. It plays a crucial role in supporting the pelvic organs, maintaining continence, and contributing to sexual function. Understanding the pelvic floor involves knowing its anatomy, function, common issues, and methods for maintaining its health.
Anatomy of the Pelvic Floor: The pelvic floor is made up of several layers of muscles and tissues that span the area between the pubic bone at the front and the coccyx (tailbone) at the back. These muscles can be categorized into three layers:
- Superficial Perineal Layer: This layer includes the bulbospongiosus and ischiocavernosus muscles. These muscles surround the openings of the vagina and urethra in women and the base of the penis in men.
- Deep Perineal Layer: This layer contains the external anal sphincter and the deep transverse perineal muscles. These muscles are responsible for maintaining control over the anus and stabilizing the pelvis.
- Pelvic Diaphragm Layer: The deepest layer consists of the levator ani muscles, which are further divided into the pubococcygeus, puborectalis, and iliococcygeus muscles. These muscles support the pelvic organs and help control urinary and fecal continence.
When is Internal Pelvic Floor Physical Therapy Needed?
Here are some situations where internal pelvic floor physical therapy might be needed:
- Pelvic Pain: Chronic pelvic pain, whether it’s related to conditions like pelvic floor muscle tension, vulvodynia, vaginismus, or other pelvic pain disorders, may benefit from internal pelvic floor therapy. The therapist can assess the muscle tension, trigger points, and any underlying issues contributing to the pain.
- Pelvic Organ Prolapse: Internal pelvic floor therapy can be helpful for individuals with pelvic organ prolapse. The therapist can teach exercises and techniques to strengthen and support the pelvic floor muscles to alleviate symptoms and improve organ positioning.
- Urinary Incontinence: If you’re experiencing urinary incontinence (leakage of urine), internal pelvic floor therapy can provide strategies to strengthen the pelvic floor muscles and improve bladder control.
- Fecal Incontinence: Individuals with fecal incontinence (involuntary bowel leakage) can benefit from internal pelvic floor therapy to strengthen the muscles that control bowel movements and improve control.
The Role of a Pelvic Floor Physical Therapist
A pelvic floor physical therapist specializes in evaluating and treating conditions related to the pelvic floor muscles and associated structures. They play a crucial role in helping individuals, both men and women, who are experiencing a range of pelvic health issues. Here’s an overview of the role of a pelvic floor physical therapist:
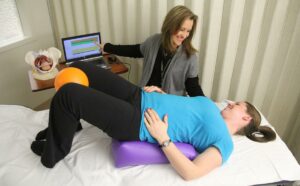
1. Assessment and Evaluation: Pelvic floor physical therapists begin by conducting a comprehensive assessment of their patients’ pelvic health. This assessment involves a thorough medical history review, discussion of symptoms and concerns, and possibly some diagnostic tests if needed. They may also perform external and internal examinations to assess muscle tone, strength, flexibility, and any potential sources of pain or dysfunction.
2. Individualized Treatment Plans: Based on the assessment findings, the pelvic floor physical therapist develops personalized treatment plans tailored to each patient’s specific needs and goals. These plans may include a combination of exercises, manual therapy techniques, behavioral modifications, and education about pelvic anatomy and function.
3. Education: Education is a significant aspect of the pelvic floor physical therapist’s role. They educate patients about the anatomy and function of the pelvic floor, how it relates to their specific condition, and what they can do to improve their pelvic health. This education empowers patients to take an active role in their recovery.
4. Pelvic Floor Exercises: Pelvic floor physical therapists teach patients how to perform pelvic floor exercises, commonly known as Kegel exercises. These exercises involve contracting and relaxing the pelvic floor muscles to strengthen them and improve their coordination. The therapist guides patients in performing these exercises correctly and monitors their progress.
Benefits of Internal Pelvic Floor Physical Therapy
Internal pelvic floor physical therapy, while it may initially seem intimidating or unfamiliar to some, offers a range of benefits for individuals dealing with various pelvic health issues. Here are some key benefits of internal pelvic floor physical therapy:
1. Accurate Assessment: Internal pelvic floor physical therapy allows for a more accurate assessment of the condition of the pelvic floor muscles and associated structures. By directly evaluating the muscles internally, the therapist can identify areas of tension, weakness, trigger points, and other issues that might not be as apparent through external examinations.
2. Personalized Treatment: The internal assessment helps the physical therapist tailor the treatment plan specifically to the individual’s needs. This personalized approach ensures that the therapy addresses the root causes of the pelvic health issue and targets areas that require improvement.
3. Targeted Muscle Training: Internal therapy allows the therapist to guide patients through exercises that specifically target the pelvic floor muscles. This guidance ensures that patients are engaging the correct muscles and performing exercises effectively, leading to better outcomes.
What to Expect During a Session
During an internal pelvic floor physical therapy session, you can expect a professional and comfortable environment where your privacy and comfort are of the utmost importance. Here’s what you can generally expect during a session:
1. Discussion of Medical History and Symptoms: The session will often start with a discussion about your medical history, current symptoms, and any concerns you might have. This helps the therapist understand your condition and tailor the session to your specific needs.
2. Privacy and Comfort: The therapist will ensure that you are comfortable and will always prioritize your privacy and dignity throughout the session. You’ll typically be provided with a private space to change and prepare for the assessment.
3. Explanation of the Process: The therapist will explain the assessment process and what will happen during the session. They will answer any questions you might have and ensure that you’re fully informed about the procedures.
Pelvic Floor Exercises and Techniques

Pelvic floor exercises, often referred to as Kegel exercises, are designed to strengthen and improve the function of the muscles in the pelvic floor. These exercises are beneficial for both men and women and can help address various pelvic health issues, such as incontinence, pelvic pain, and sexual dysfunction. Here’s a guide to pelvic floor exercises and techniques:
1. Basic Pelvic Floor Muscle Contraction (Kegels): The fundamental pelvic floor exercise involves contracting and relaxing the pelvic floor muscles. Here’s how to perform a basic Kegel exercise:
- Sit, stand, or lie down comfortably.
- Identify the muscles you use to stop the flow of urine or prevent passing gas. These are your pelvic floor muscles.
- Contract these muscles by squeezing them as if you’re trying to hold back urine or gas.
- Hold the contraction for a few seconds (start with 3-5 seconds) and then release.
- Relax the muscles completely after the contraction.
- Perform 10-15 repetitions, gradually increasing the duration of the contractions over time.
2. Gradual Muscle Contractions: In addition to the basic Kegel exercise, you can practice gradual muscle contractions to strengthen different muscle fibers within the pelvic floor:
- Squeeze your pelvic floor muscles gently.
- Gradually increase the intensity of the contraction, as if you’re lifting an elevator from the ground floor to the first floor, then to the second floor (increasing the squeeze with each floor).
- Hold the contraction for a few seconds at maximum intensity.
- Gradually release the contraction as if the elevator is descending.
- Perform 10-15 repetitions of these gradual contractions.
Fast Twitch Contractions: These exercises focus on quickly contracting and relaxing the pelvic floor muscles. They simulate the rapid contractions that occur during activities like coughing or sneezing:
- Contract your pelvic floor muscles quickly and forcefully.
- Release the contraction immediately.
- Perform 10-15 repetitions of fast contractions.
Deep Breathing and Relaxation: Breathing and relaxation techniques are important to complement pelvic floor exercises:
- Breathe deeply and fully into your diaphragm.
- As you exhale, gently contract your pelvic floor muscles.
- As you inhale, relax the pelvic floor muscles.
- This technique helps coordinate breathing and muscle engagement for optimal pelvic floor function.
Preparing for Your First Appointment

Preparing for your first pelvic floor physical therapy appointment involves a combination of practical and mental preparation to ensure you’re comfortable and ready for the session. Here are some steps to help you prepare:
1. Gather Information:
- Make a list of your symptoms, concerns, and questions. This will help you communicate effectively with the therapist about your condition and what you’re experiencing.
- Gather any relevant medical records, test results, or documents related to your pelvic health.
2. Research and Choose a Qualified Therapist:
- Ensure that the therapist you’re seeing is qualified and experienced in pelvic floor physical therapy. Check their credentials and reviews.
- If you have any specific concerns or needs, find a therapist who specializes in those areas.
3. Wear Comfortable Clothing:
- Wear comfortable, loose-fitting clothing that you can easily move in. You may need to change into a gown or appropriate attire for the assessment.
Conclusion
In the grand tapestry of our health, the pelvic floor holds a significant thread. From supporting our organs to facilitating pleasurable experiences, its role cannot be underestimated. Internal pelvic floor physical therapy offers a targeted and effective way to address a wide range of concerns, ultimately improving quality of life. So, whether you’re a new mom seeking postpartum recovery or an individual striving for enhanced pelvic wellness, consider embracing the potential benefits of internal pelvic floor therapy.
Physical Therapy helps patients recover from pain. If you’re experiencing Back, Shoulder, Knee, Neck, Elbow, Hip, or Arthritis pain, a physical therapist at PhysioMantra can help: Book an online physical therapy session.



