Jumper’s knee, medically known as patellar tendinitis, is a common ailment among individuals who engage in activities that involve repetitive jumping and explosive movements. While it predominantly affects athletes, it can also impact anyone who participates in high-impact sports or has an active lifestyle. This article aims to provide insights into jumper’s knee, its causes, symptoms, and various treatment options available for effective pain relief and recovery.
Contents
Understanding Jumper’s Knee
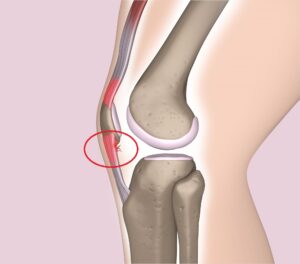
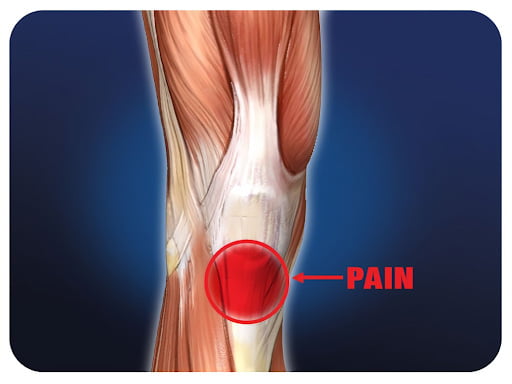
Jumper’s knee is characterized by pain and inflammation in the patellar tendon, which connects the kneecap to the shinbone. Jumper’s knee, also known as patellar tendinopathy or patellar tendonitis, is a common overuse injury that affects the patellar tendon connecting the patella (kneecap) to the tibia (shinbone).
It is frequently seen in athletes who engage in activities that involve repetitive jumping and explosive movements, such as basketball, volleyball, and track and field events.
Symptoms of Jumper’s Knee
Symptoms of jumper’s knee, also known as patellar tendinopathy or patellar tendonitis, can vary in severity but generally revolve around pain and discomfort in the area around the patellar tendon, which connects the patella (kneecap) to the tibia (shinbone). Here are the common symptoms associated with jumper’s knee:
- Pain Below the Kneecap: The hallmark symptom of a jumper’s knee is pain located just below the kneecap. This pain is often described as aching, sharp, or stabbing. It might start off as a mild discomfort but can progress to more pronounced pain with continued activity.
- Pain with Activity: The pain is usually exacerbated by activities that involve bending the knee, such as jumping, landing, running, squatting, and climbing stairs. Repetitive movements and high-impact activities tend to worsen the pain.
- Tenderness and Swelling: There might be tenderness and swelling around the area where the patellar tendon attaches to the shinbone. The tendon itself might feel tender to the touch.
- Stiffness: Some individuals with jumper’s knee may experience stiffness in the knee, especially after periods of inactivity or upon waking up in the morning.
- Gradual Onset: Jumper’s knee symptoms tend to develop gradually over time due to the repetitive stress on the patellar tendon. The pain might be mild initially and become more noticeable as the condition progresses.
- Pain Relief with Rest: Resting the affected knee can lead to a reduction in pain. However, once the individual resumes high-impact activities, the pain may return.
Risk Factors of Jumper’s Knee

Several factors can increase the risk of developing a jumper’s knee, also known as patellar tendinopathy or patellar tendonitis. These factors can contribute to the overuse and strain on the patellar tendon, leading to the development of the condition. Here are some common risk factors:
- High-Impact Activities: Engaging in sports and activities that involve repetitive jumping, sudden changes in direction, and explosive movements can increase the risk of a jumper’s knee. Sports like basketball, volleyball, track and field events, and gymnastics put significant stress on the patellar tendon.
- Overuse and Intense Training: Overtraining without adequate rest and recovery can lead to excessive strain on the patellar tendon. Intense training regimens that don’t allow enough time for the tendon to heal and adapt can increase the risk of injury.
- Sudden Increase in Activity: Rapidly increasing the intensity, duration, or frequency of physical activities without giving the body time to adjust can lead to a jumper’s knee. Gradual progression is important to allow the tendon to adapt to new demands.
- Muscle Imbalances: Weakness or imbalances in the quadriceps and hamstring muscles can alter the mechanics of the knee joint and increase the load on the patellar tendon during movement.
- Poor Biomechanics: Abnormal movement patterns or poor jumping and landing techniques can lead to excessive stress on the patellar tendon. These biomechanical issues can be caused by factors such as flat feet, tight muscles, and poor body alignment.
Prevention Strategies for Jumper’s Knee
Preventing a jumper’s knee, also known as patellar tendinopathy or patellar tendonitis, involves a combination of strategies that focus on reducing the risk of overuse and strain on the patellar tendon. Here are some effective prevention strategies:
Proper Technique and Biomechanics:
- Learn and practice proper jumping, landing, and movement techniques to minimize stress on the patellar tendon.
- Focus on maintaining good body alignment during movements to avoid excessive strain on the knee joint.
Gradual Progression:
- Gradually increase the intensity, duration, and frequency of activities that involve jumping and explosive movements.
- Avoid sudden spikes in training volume or intensity that can lead to overuse injuries.
Cross-Training:
- Engage in a variety of physical activities to reduce the repetitive stress on the same muscle groups and tendons.
- Incorporate low-impact activities like swimming, cycling, and yoga into your routine.
Strength and Flexibility:
- Build and maintain balanced muscle strength, especially in the quadriceps, hamstrings, and calf muscles.
- Include targeted strength training exercises for the lower body in your fitness regimen.
- Prioritize flexibility exercises to maintain a good range of motion in the knee joint and surrounding muscles.
Warm-Up and Cool-Down:
- Always start your workouts with a proper warm-up that includes light aerobic activity and dynamic stretches to prepare the muscles and tendons for exercise.
- End your sessions with a cool-down that includes static stretches to improve flexibility and aid in recovery.
- Conservative Treatments
Medications for Pain and Inflammation
Over-the-counter pain relievers such as ibuprofen can temporarily alleviate pain and reduce inflammation. Nonsteroidal anti-
Here are some common types of medications used for pain and inflammation:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- Examples: Ibuprofen (Advil, Motrin), Naproxen (Aleve), Aspirin
- NSAIDs are commonly used to relieve pain, reduce inflammation, and lower fever. They work by blocking certain enzymes that contribute to inflammation.
- These medications can help manage pain and discomfort associated with jumper’s knee, but prolonged or excessive use should be avoided due to potential side effects on the stomach and kidneys.
Topical Analgesics:
- Examples: Topical NSAID creams, Capsaicin cream, Lidocaine patches
- These creams, gels, or patches are applied directly to the skin over the painful area. They can provide localized pain relief without affecting the entire body as oral medications might.
Acetaminophen:
- Example: Tylenol
- Acetaminophen is an over-the-counter pain reliever that can help manage mild to moderate pain. Unlike NSAIDs, it does not have anti-inflammatory properties. It’s important not to exceed the recommended dosage to avoid potential liver damage.
Advanced Treatment Options
Here are some advanced treatment options for jumper’s knee:
Platelet-Rich Plasma (PRP) Therapy:
- PRP therapy involves taking a small amount of the patient’s blood, processing it to concentrate the platelets (which contain growth factors), and then injecting the platelet-rich solution into the affected area.
- The growth factors in PRP are believed to stimulate the body’s natural healing processes and promote tissue regeneration.
Extracorporeal Shockwave Therapy (ESWT):
- ESWT is a non-invasive procedure that uses shockwaves to stimulate blood flow, enhance healing, and reduce pain in the affected area.
- It’s thought that the shockwaves break down scar tissue and stimulate the body’s natural repair mechanisms.
Prolotherapy:
- Prolotherapy involves injecting a solution, often containing a dextrose solution, into the affected area to stimulate inflammation and trigger the body’s healing response.
- The goal is to strengthen the damaged tissues and promote healing through the creation of new collagen fibers.
Ultrasound-Guided Injections:
- Injections of medications, such as corticosteroids or other substances, can be delivered with greater precision using ultrasound guidance.
- This ensures that the medication is accurately placed in the target area
Surgery (Tenotomy or Tenodesis):
- Surgical intervention is generally considered a last resort for a jumper’s knee when conservative treatments have failed or if the condition is severe and significantly impacts the individual’s quality of life.
- Surgical options may include tenotomy (partial or complete removal of the damaged tendon) or stenosis (reattaching the tendon to a different part of the bone).
Rehabilitation and Recovery

Rehabilitation and recovery are critical aspects of managing a jumper’s knee (patellar tendinopathy) and restoring optimal function to the affected knee. A comprehensive rehabilitation program aims to reduce pain, strengthen the muscles around the knee, improve flexibility, and gradually reintroduce physical activity. Here are the key components of rehabilitation and recovery for a jumper’s knee:
- Professional Guidance: Work with a sports medicine specialist or physical therapist who has experience in treating tendon injuries. They can create a tailored rehabilitation plan based on your specific condition, needs, and goals.
- Initial Rest: Depending on the severity of your symptoms, a period of rest may be recommended to allow the damaged tendon to heal. During this time, avoid activities that exacerbate pain.
- Pain Management: In the early stages, pain relief strategies such as ice application, elevation, and over-the-counter pain medications may help manage discomfort.
- Flexibility and Mobility: Gentle stretching and mobility exercises for the quadriceps, hamstrings, calf muscles, and hip flexors can help maintain or improve joint range of motion.
- Biomechanical Analysis: A physical therapist can assess your movement patterns and identify any biomechanical issues that contribute to the condition. Addressing these issues can reduce strain on the patellar tendon.
Conclusion
Jumper’s knee can significantly impact an individual’s quality of life, especially for those who lead active lifestyles. Recognizing the symptoms, seeking timely medical attention, and following a comprehensive treatment plan are key to managing the condition effectively. By adopting preventive measures, adhering to treatment guidelines, and staying informed about advancements, individuals can successfully overcome jumper’s knee and return to their favorite activities.
If you’re experiencing Knee pain, physical therapy for knee pain at PhysioMantra can help: Book an online physical therapy session.