Osgood-Schlatter Disease is more than just a mouthful of words – it’s a condition that can cause real discomfort and hinder an active lifestyle. But fear not, because the road to recovery is paved with the powerful tools of physical therapy. In this article, we’ll delve into the world of Osgood-Schlatter Disease, understand its nuances, and explore how physical therapy can make a significant difference in managing the condition.
Contents
Understanding Osgood-Schlatter Disease
Osgood-Schlatter Disease, often referred to as OSD, is a common condition that primarily affects adolescents undergoing growth spurts. It involves inflammation of the patellar tendon which attaches to the shinbone, resulting in pain and swelling below the knee.
This condition most frequently occurs in active individuals, particularly those engaged in sports that involve running, jumping, and swift changes in direction.
Symptoms of Osgood-Schlatter Disease
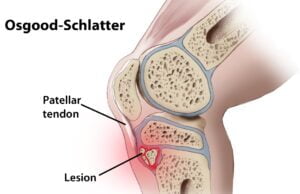
Osgood-Schlatter disease, also known as OSD or Osgood-Schlatter syndrome, is a condition that primarily affects adolescents, especially those who are physically active and participate in sports that involve running, jumping, and rapid changes in direction. It is characterized by inflammation and pain at the point where the patellar tendon attaches to the tibia (shinbone), just below the kneecap. This condition usually occurs during periods of rapid growth.
Common symptoms of Osgood-Schlatter disease include:
- Knee Pain: Pain is the most prominent symptom of OSD. The pain is typically felt just below the kneecap and can range from mild discomfort to more severe pain. The pain often worsens with physical activity and can improve with rest.
- Swelling: There may be swelling and tenderness at the site where the patellar tendon attaches to the tibia. This can result in a visible bump or prominence just below the kneecap.
- Limited Mobility: The affected knee may have reduced flexibility and movement due to pain and inflammation.
- Worsening Pain with Activity: Activities that involve running, jumping, squatting, or kneeling can exacerbate the pain. Adolescents who are active in sports are more likely to experience this pain during or after physical activity.
- Pain Aggravation with Pressure: Applying pressure to the affected area or contracting the quadriceps muscles (such as by straightening the knee) can cause increased pain.
- Tightness of Quadriceps Muscles: The muscles in the front of the thigh (quadriceps) may become tight and tense due to the inflammation and stress on the patellar tendon.
Who is Most Susceptible to the Condition?
Osgood-Schlatter disease primarily affects adolescents, particularly those who are active in sports and physical activities. While it can occur in both genders, certain groups are more susceptible to developing the condition:
- Age: Osgood-Schlatter disease typically occurs during periods of rapid growth, which commonly happens during early adolescence. Boys usually experience growth spurts between the ages of 10 and 15, while girls experience them between the ages of 8 and 13. As a result, these age ranges are when the risk of developing OSD is highest.
- Gender: Boys are more commonly affected by Osgood-Schlatter disease than girls. This could be due to differences in growth rates, muscle development, and activity levels between the two genders.
- Physically Active Individuals: Adolescents who are highly active in sports and activities that involve running, jumping, squatting, and other movements that stress the knee joint are more susceptible. The repetitive stress on the patellar tendon insertion site during these activities can contribute to the development of OSD.
- Rapid Growers: Those who experience rapid growth spurts are more at risk. When bones grow rapidly, they may outpace the development of muscles and tendons, leading to increased tension and stress at the patellar tendon attachment point.
- Muscle Imbalances: Individuals with imbalances in muscle strength and flexibility around the knee joint are more likely to develop OSD. Tight quadriceps muscles and weak hamstrings or hip muscles can contribute to this imbalance.
- Biomechanical Factors: People with certain biomechanical factors that affect knee joint alignment and movement might be more susceptible to OSD. For instance, issues with knee alignment, foot pronation, or gait abnormalities can increase the risk.
- Genetic Predisposition: While not fully understood, genetics might play a role in determining susceptibility to OSD. Some individuals may have a genetic predisposition that makes them more likely to develop the condition.
The Role of Physical Therapy

Physical therapy plays a pivotal role in managing OSD. Its tailored exercises and techniques help alleviate pain, strengthen muscles, and improve flexibility. Moreover, physical therapy promotes proper healing and prevents future complications, allowing individuals to return to their activities with confidence.
Physical therapy aims to achieve several goals, including pain reduction, improvement in joint mobility, enhanced muscle strength, and the restoration of functional movement. It also educates patients about correct posture and body mechanics to prevent further strain.
Assessment and Diagnosis
The assessment and diagnosis of Osgood-Schlatter disease typically involve a combination of medical history, physical examination, and, in some cases, imaging studies. Here’s how the process usually unfolds:
- Medical History: The healthcare provider will begin by asking about the patient’s medical history, including any history of recent growth spurts, physical activities, sports participation, and the nature of the knee pain. This information helps to establish a context for the symptoms.
- Physical Examination: A thorough physical examination of the affected knee is crucial. The healthcare provider will look for signs such as swelling, tenderness, and the presence of a bony bump just below the kneecap (which is characteristic of Osgood-Schlatter disease). They will also assess the knee’s range of motion, muscle strength, and any pain elicited during specific movements.
- Palpation: The healthcare provider may gently press and feel the area just below the kneecap to identify points of tenderness and evaluate the condition of the patellar tendon insertion.
- Functional Tests: Certain functional tests, such as squatting or extending the knee against resistance, may be performed to assess pain and discomfort during movement.
- Imaging Studies: In some cases, imaging studies like X-rays or ultrasound may be ordered. These imaging techniques can help rule out other potential causes of knee pain and confirm the presence of changes characteristic of Osgood-Schlatter disease, such as inflammation at the patellar tendon insertion point or bony changes in the tibial tuberosity (the bump below the kneecap).
Treatment of Osgood-Schlatter Disease

The treatment of Osgood-Schlatter disease (OSD) focuses on managing symptoms, reducing pain and discomfort, and allowing the condition to naturally resolve as the individual completes their growth spurt. Here are some common treatment strategies:
- Rest: Avoiding or reducing activities that exacerbate pain and discomfort is important. This doesn’t necessarily mean complete rest, but rather modifying activities to minimize strain on the knee joint. Low-impact exercises like swimming might be a good alternative during this time.
- Ice: Applying ice to the affected area for 15-20 minutes every 2-3 hours can help reduce inflammation and alleviate pain. Make sure to use a cloth or towel to protect the skin from direct contact with ice.
- Pain Relief: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, can be used under the guidance of a healthcare professional to manage pain and inflammation
- Knee Brace or Strap: Some individuals find relief by using a knee brace or strap that supports the patellar tendon and reduces stress on the affected area.
- Heel Cord Stretching: Stretching the calf muscles and Achilles tendon can help reduce tension on the patellar tendon insertion point. Gentle stretching exercises can be recommended by a healthcare provider or physical therapist.
- Gradual Return to Activity: As symptoms improve, gradually returning to physical activities can be done. However, it’s important to monitor for any discomfort and to progress slowly to avoid exacerbating the condition.
- Time: OSD is a self-limiting condition that usually improves and resolves as the individual’s growth spurt concludes and bones and muscles mature. Most adolescents will see a significant reduction in symptoms by their late teens.
- Medical Monitoring: Regular follow-up with a healthcare provider, such as a pediatrician or orthopedic specialist, is recommended to track progress and ensure that the condition is improving as expected.
Surgery is rarely needed for Osgood-Schlatter disease. In severe cases where pain persists and other conservative measures have not provided relief, a surgical option might be considered, but this is a rare scenario.
Conclusion
In conclusion, Osgood-Schlatter Disease might be a hurdle, but with the right tools and guidance, it’s a hurdle that can be overcome. Physical therapy emerges as a powerful ally in managing the condition, providing a pathway to reduced pain, enhanced mobility, and a return to an active lifestyle. So, whether you’re a young athlete or an adult seeking relief, remember that the journey to recovery starts with a step – a step towards comprehensive physical therapy.
If you’re experiencing Knee pain, physical therapy for knee pain at PhysioMantra can help: Book an online physical therapy session.



