The human body’s intricate network of joints enables us to perform a wide range of movements, and the acromioclavicular joint is no exception. Located at the top of the shoulder, this joint connects the collarbone (clavicle) to the shoulder blade (scapula). Over time, due to factors like wear and tear and the natural aging process, this joint can develop a condition known as Acromioclavicular Joint Arthritis, causing pain, inflammation, and reduced range of motion. In this comprehensive guide, we’ll delve into the intricacies of AC joint arthritis, its causes, and symptoms, as well as various treatment and management options.
Contents
Understanding the Acromioclavicular Joint
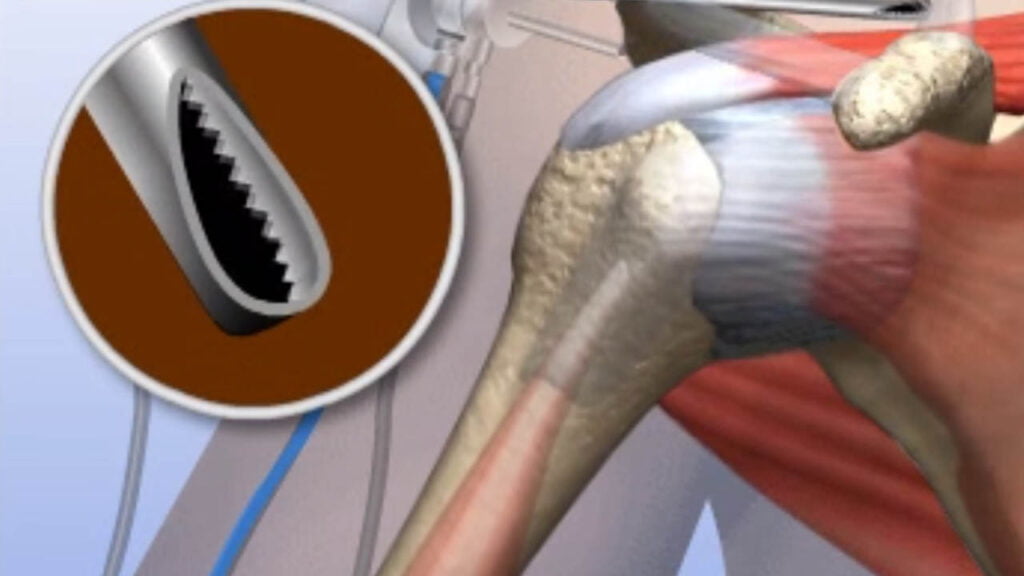
This joint is integral in providing support and stability to the shoulder, especially during overhead movements. It consists of cartilage, ligaments, and synovial fluid that facilitate smooth gliding of the bones.
AC joint arthritis is a degenerative condition that primarily affects the acromioclavicular joint. This joint, crucial for shoulder and arm movement, is susceptible to the same wear and tear that can affect other joints in the body. The gradual breakdown of the cartilage that cushions the joint’s movement leads to friction between bones, resulting in pain, swelling, and inflammation.
Causes and Risk Factors of Acromioclavicular Joint Arthritis
Acromioclavicular Joint Arthritis, a condition characterized by the degeneration of the AC joint connecting the collarbone and the shoulder blade, can arise from a combination of factors. Understanding the causes and risk factors can help individuals recognize the potential for developing this condition and take appropriate measures. Here, we delve into the key contributors to AC joint arthritis:
- Degenerative Changes: The primary cause of AC joint arthritis is the natural degeneration of joint structures over time. As we age, the protective cartilage covering the ends of bones in the joint gradually wears away, leading to friction and inflammation.
- Injury or Trauma: Previous shoulder injuries, especially those affecting the AC joint directly, can contribute to the development of arthritis. Trauma or fractures around the AC joint can disrupt the joint’s integrity and accelerate degenerative changes.
- Repetitive Strain: Engaging in activities that involve repetitive overhead motions, such as weightlifting, throwing sports, or certain occupations like painting, can increase the stress on the AC joint. Over time, this repetitive strain can lead to joint breakdown.
- Genetic Predisposition: Genetics play a role in determining an individual’s susceptibility to arthritis. Some people might have genetic factors that make them more prone to joint degeneration.
- Postural Issues: Poor posture and incorrect shoulder mechanics can place excessive stress on the AC joint, hastening its degeneration. Long-term poor posture can lead to joint imbalances and uneven wear.
Signs and Symptoms of Acromioclavicular Joint Arthritis
Acromioclavicular Joint Arthritis can manifest through a range of signs and symptoms, often affecting the shoulder’s mobility and causing discomfort. Recognizing these indicators is crucial for seeking timely medical attention and appropriate management. Here are the key signs and symptoms associated with AC joint arthritis:
- Pain: Persistent or intermittent pain is one of the most common symptoms of AC joint arthritis. The pain is typically localized at the top of the shoulder, near the AC joint. It may range from a dull ache to sharp pain, and it can worsen with certain movements or activities that involve raising the arm overhead, lifting, or reaching across the body.
- Swelling: Inflammation of the AC joint can lead to noticeable swelling around the joint area. The swelling might be accompanied by redness and warmth.
- Tenderness: When touched, the area around the AC joint may feel tender or sensitive. Pressing on the joint or surrounding tissues can elicit discomfort.
- Reduced Range of Motion: AC joint arthritis can limit the shoulder’s range of motion. Individuals may experience difficulty when trying to raise the arm fully, rotate it, or engage in activities requiring extensive shoulder movement.
- Crepitus: Crepitus refers to a sensation of grinding, clicking, or popping within the joint when it’s moved. This sensation is caused by the rough surfaces of bones rubbing against each other due to the loss of protective cartilage.
Diagnosing Acromioclavicular Joint Arthritis
Diagnosing Acromioclavicular (AC) Joint Arthritis involves a combination of clinical evaluation, medical history assessment, physical examination, and often imaging studies. A healthcare professional, usually an orthopedic specialist or a rheumatologist, will perform these steps to accurately diagnose the condition. Here’s a detailed overview of the diagnostic process for AC joint arthritis:
1. Medical History: The healthcare provider will begin by gathering information about your symptoms, medical history, and any previous shoulder injuries or conditions. They will inquire about the onset of pain, the nature of discomfort, and any activities that worsen or alleviate the symptoms.
2. Physical Examination: During the physical examination, the healthcare provider will:
- Palpate the AC joint area to identify tenderness, swelling, or other abnormalities.
- Assess your shoulder’s range of motion and any limitations.
- Perform specific maneuvers to reproduce the pain or crepitus associated with AC joint arthritis.
3. Imaging Studies: Imaging tests are often necessary to confirm the diagnosis and assess the extent of joint degeneration. The following imaging modalities can aid in diagnosing AC joint arthritis:
- X-rays: X-rays provide detailed images of bone structures. They can reveal narrowing of the joint space, changes in bone density, and the presence of bone spurs or other degenerative changes characteristic of arthritis.
- MRI (Magnetic Resonance Imaging): MRI scans provide a more detailed view of soft tissues, such as cartilage, ligaments, and tendons. An MRI can help assess the condition of the cartilage in the AC joint and identify any associated tissue damage.
- Ultrasound: Ultrasound can be used to visualize soft tissues and can help detect inflammation and other abnormalities around the AC joint.
- CT Scan (Computed Tomography): CT scans offer cross-sectional images of the joint, providing more detailed information about bone structures and joint alignment.
Conservative Treatment Options
Conservative treatment options play a crucial role in managing Acromioclavicular (AC) Joint Arthritis, especially in the early stages of the condition. These approaches focus on relieving pain, reducing inflammation, improving joint function, and enhancing the individual’s quality of life.
It’s important to note that the effectiveness of these treatments can vary based on the severity of the arthritis and the individual’s response. Here are some common conservative treatment options for AC joint arthritis:
1. Rest and Activity Modification: Resting the affected shoulder and avoiding activities that exacerbate pain can help reduce stress on the AC joint. Modifying or adjusting the way you perform certain tasks can also minimize joint strain.
2. Physical Therapy: A physical therapist can design a tailored exercise program to strengthen the muscles around the shoulder joint, improve range of motion, and enhance joint stability. Exercises might include stretching, strengthening, and postural correction routines.
3. Pain Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help alleviate pain and reduce inflammation. Always consult a healthcare professional before starting any medication regimen.
4. Ice and Heat Therapy: Applying ice packs to the affected area can help reduce pain and inflammation, especially after activities that worsen symptoms. Heat therapy, such as warm compresses or heat packs, can promote relaxation and improve blood flow.
5. Assistive Devices: Using assistive devices such as slings or braces can provide support and limit movement in the affected shoulder, allowing it to rest and heal.
6. Corticosteroid Injections: Medical professionals may administer corticosteroid injections directly into the AC joint to provide short-term pain relief by reducing inflammation. These injections should be used cautiously and sparingly due to potential side effects.
7. Topical Treatments: Topical creams or gels containing analgesic or anti-inflammatory agents can be applied directly to the skin over the affected joint for localized relief.
8. Lifestyle Modifications: Adopting ergonomic practices and maintaining good posture can reduce unnecessary stress on the AC joint during daily activities.
Conclusion
Acromioclavicular joint arthritis can significantly impact an individual’s quality of life, affecting their ability to perform everyday tasks and enjoy activities they love. However, with timely diagnosis, appropriate medical interventions, and lifestyle modifications, managing the condition is possible. By staying informed and seeking professional guidance, individuals can take proactive steps toward a healthier, more comfortable life.
If you’re experiencing Shoulder pain, physical therapy for shoulder pain at PhysioMantra can help: Book an online physical therapy session.