Every step feels like a reminder, a nudge to a persistent discomfort that keeps echoing from the hip. Osteoporosis hip pain isn’t just another ailment; it’s a silent whisper of weakening bones, often going unnoticed until it’s severe. If you’ve ever wondered why the pain is more pronounced with certain movements, or why the ache doesn’t seem to subside with general pain relief methods, you’re not alone. Dive deep with us as we break down the enigma of osteoporosis hip pain, unveiling its causes and charting a path to effective solutions.
Contents
Understanding Osteoporosis: A Brief Overview
Osteoporosis, derived from the Greek words ‘osteo‘ (bone) and ‘porosis‘ (passage or pore), translates to ‘porous bone’. It’s a condition characterized by a decrease in bone density, leading to fragile bones that are more prone to fractures. Those particularly at risk include post-menopausal women, elderly individuals, and those with a family history of the disease. But what’s most daunting about osteoporosis is its silent nature. Often, it progresses without any noticeable symptoms until a sudden strain, bump, or fall causes a fracture. This stealthy behavior has earned it the moniker ‘silent disease’, emphasizing the importance of early detection and proactive care.
How Osteoporosis Affects the Hip?
 The hip, a ball-and-socket joint, plays a pivotal role in our body’s mobility. It’s formed where the femur (thigh bone) meets the pelvis, creating a robust joint designed to withstand wear and tear. But when osteoporosis sets in, this once-sturdy structure becomes vulnerable.
The hip, a ball-and-socket joint, plays a pivotal role in our body’s mobility. It’s formed where the femur (thigh bone) meets the pelvis, creating a robust joint designed to withstand wear and tear. But when osteoporosis sets in, this once-sturdy structure becomes vulnerable.
Osteoporosis results in a reduction of bone mineral density. As the hip bones become less dense and more porous, they lose their strength and resilience. This weakening is particularly concerning for the hip, given the substantial weight and force it supports during activities like walking, standing, or even sitting.
As osteoporosis progresses, the hip bone’s weakened state makes it increasingly susceptible to fractures, even from minor incidents like a minor trip or sudden twist. These fractures can lead to intense pain, restricted movement, and in severe cases, surgical interventions like hip replacements.
Beyond fractures, the gradual loss of bone density can lead to chronic pain in the hip area, resulting from the joint’s decreased stability and the muscles and tendons overcompensating for the bone’s weakness.
In essence, while the hip is designed for durability, osteoporosis presents a significant challenge, compromising its strength and function.
Factors Contributing to Osteoporosis Hip Pain
 Understanding osteoporosis hip pain involves recognizing the myriad factors that contribute to its onset and progression. Here’s a rundown of key contributors:
Understanding osteoporosis hip pain involves recognizing the myriad factors that contribute to its onset and progression. Here’s a rundown of key contributors:
- Age: As we age, our bones naturally lose density, making older individuals more susceptible to osteoporosis.
- Genetics: A family history of osteoporosis can increase one’s risk, suggesting a genetic predisposition to the condition.
- Lifestyle Choices:
- Diet: Insufficient calcium and vitamin D intake can hinder bone strength and repair.
- Physical Activity: A sedentary lifestyle can accelerate bone density loss.
- Tobacco and Alcohol: Excessive consumption can interfere with the body’s ability to absorb calcium and weaken bones.
- Hormonal Changes:
- Menopause: The decline in estrogen levels post-menopause can hasten bone loss.
- Thyroid: Overactive thyroid or prolonged use of thyroid medication can contribute to bone density reduction.
- Medications and Other Conditions: Certain medications, like corticosteroids, or medical conditions, such as rheumatoid arthritis and certain digestive disorders, can heighten the risk of osteoporosis.
- Gender: Women, especially those who’ve reached menopause, are at a higher risk due to thinner bones and the drop in estrogen levels.
Each of these factors, either in isolation or combined, plays a role in determining an individual’s susceptibility to osteoporosis hip pain. Recognizing and addressing them can pave the way for prevention and effective management.
Treatment Options for Osteoporosis-Driven Hip Pain

Managing and mitigating osteoporosis hip pain is paramount to preserving mobility and overall quality of life. Thankfully, a myriad of treatment options exists, catering to varying degrees of severity and individual needs:
Medications
- Bisphosphonates: These are the most common medications prescribed for osteoporosis, helping to prevent bone loss and reduce fracture risk.
- Hormone Replacement Therapy (HRT): Especially for post-menopausal women, HRT can help maintain bone density. However, it’s essential to discuss potential risks and benefits with a doctor.
- Selective Estrogen Receptor Modulators (SERMs): Medications like raloxifene mimic estrogen’s bone-saving effects without affecting other tissues.
- Bone-Building Medications: Drugs like teriparatide can stimulate bone formation, albeit they’re usually reserved for severe cases due to side effects and cost.
Physical Therapy
- Targeted Exercises: Special exercises can strengthen the muscles surrounding the hip, reducing pain and improving stability.
- Mobility Training: Techniques to improve balance and gait can be taught, minimizing the risk of falls.
- Pain Management Techniques: Modalities like heat, cold, and ultrasound can be used to alleviate pain and improve function.
Lifestyle Modifications
- Diet: Boosting calcium and vitamin D intake either through diet or supplements ensures bones get essential nutrients.
- Weight-bearing Exercises: Activities like walking, jogging, or dancing can help maintain bone density.
- Limiting Alcohol and Tobacco: Moderation can prevent further weakening of bones and improve overall health.
Surgical Interventions
- Hip Fracture Repair: In the event of a fracture, surgical pins, screws, or plates might be needed to stabilize the hip.
- Hip Replacement: For severe damage or persistent pain, a prosthetic hip joint might be considered.
Selecting the best treatment pathway requires a comprehensive evaluation and discussion with healthcare professionals. Personalized treatment plans can effectively manage symptoms and prevent further deterioration.
Physical Therapy and Exercises for Strengthening the Hip
Physical therapy plays an instrumental role in managing osteoporosis hip pain, focusing on strengthening the surrounding musculature, improving balance, and increasing bone density. Here are some effective exercises tailored to bolster the hip:
Clamshells
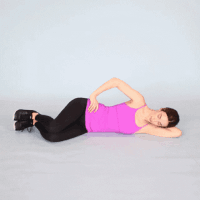
Lie on one side with legs bent at a 90-degree angle, feet together.
- Keep your heels together.
- Open and close the knees without moving the pelvis.
- Perform 10-15 repetitions, then switch sides.
Bridging

Lying on your back with knees bent, feet flat on the floor.
- Lift the hips towards the ceiling, squeezing the glutes.
- Hold for a few seconds, then lower back down.
- Repeat 10-15 times.
Standing Leg Lifts

Stand straight, holding onto a sturdy chair or counter for support.
- Slowly lift one leg out to the side without tilting your torso.
- Hold for a moment, then lower back down.
- Do 10-15 repetitions on each side.
Hip Abduction with Resistance Band

Sit on a chair with a resistance band tied around your thighs.
- Spread your legs apart against the resistance of the band.
- Return to the starting position.
- Complete 10-15 repetitions.
Hip Flexor Stretches

Begin in a lunge position with one foot forward.
- Push the hips forward gently, feeling a stretch in the front of the hip of the back leg.
- Hold for 20-30 seconds, then switch sides.
Seated Marching

Sit on a chair with feet flat on the ground.
- Lift one knee towards the chest, then lower.
- Alternate legs, mimicking a marching motion.
- Continue for 1-2 minutes.
Incorporating these exercises into a regular routine can significantly benefit those with osteoporosis hip pain. However, it’s essential to consult a physical therapist or physician before starting any new exercise regimen to ensure safety and effectiveness.
Tips for Daily Care
For those managing osteoporosis hip pain, simple daily practices can make a world of difference in preventing further deterioration and ensuring overall well-being. Here’s a set of handy tips tailored for daily care:
- Stay Active: Regular low-impact exercises like walking, swimming, or cycling can help maintain bone density and improve overall joint health.
- Mind Your Diet: Ensure an adequate intake of calcium and vitamin D, which are essential for bone health. Dairy products, leafy greens, and fortified foods are great sources.
- Avoid Smoking and Limit Alcohol: Both can decrease bone density and increase the risk of fractures.
- Practice Safe Movements: Avoid bending forward from the waist and twisting the spine, which can risk fractures. Use proper body mechanics when lifting.
- Use Assistive Devices if Needed: Walking aids or grab bars in bathrooms can help prevent falls and offer support.
- Wear Supportive Footwear: Proper shoes can improve balance, reduce the risk of slipping, and offer cushioning against shocks.
- Watch Your Posture: Standing and sitting upright can distribute weight evenly and reduce undue stress on the hip and spine.
- Bone Density Testing: Regular screenings can help monitor bone density and adjust treatments as needed.
Prioritizing these daily care tips can significantly minimize the risk of osteoporosis-related hip pain and improve the overall quality of life.
Conclusion
Osteoporosis hip pain can undoubtedly be a challenging and limiting condition, but armed with the right knowledge and tools, one can navigate its intricacies and live a fulfilling life. By understanding the disease, practicing daily care routines, and staying proactive, you not only manage pain but also mitigate further risks.
If you’re experiencing hip pain, there’s no need to endure it silently. At PhysioMantra, our team of dedicated professionals can guide you through specialized physical therapy for hip pain arising from osteoporosis. Don’t let pain define your life. Book an online physical therapy session with PhysioMantra today and embark on your journey to relief and recovery.



